This is the ongoing chronicle of Me, a PKD Patient: Part 1~ April, 2006 until March 5, 2009 on dialysis and blogging my adventures as a participant, and Part 2~ My Kidney Transplant on March 9, 2009 and blogging my adventures in healing and adjusting to Mordechai the Miracle Kidney and integrating this all into my life.
5/24/06
14) The Early Shift
El Milagro: I got here at 5:30 am! There were already a number of people cannulated and the place was jumping. All the nurses and techs were busy with patients and I had to wait about 20 minutes for Debbie to start on me. Now, this was a bit annoying, since I said I¹d be at work by 10 am. I¹m sitting here realizing that when I come in for dialysis in the afternoon, it doesn¹t really matter how long the whole process takes, since I¹m just going home afterwards. Coming in before work is already making me feel the anxiety of having to get to work by a certain time, so let¹s get this thing going. Debbie finished cannulating me at 5:50, adding 20 minutes to my 4 hours.
It seemed that every single thing that could happen to slow the process down happened today. I was able to fall back asleep and slept until about 8:30. Around 9 I started feeling very clammy and faint and James came over and said my blood pressure was way down (75/56) and he began giving me saline to raise it. That was another 20 minutes added to my time. I finished the session and James pulled the needles and put gauze on the holes for me to hold until they began to clot. I held them for about seven minutes, and then Debbie came by to tape them up. She peeked at the arterial hole and it spurted blood about a foot and a half, so she clamped it and that added another 8 minutes or so. This added time wouldn't worry me if I was going home, but like I said, I still have my workday ahead of me.
Data Notes: In @ 70.6 and out @ 70.1
The Rest of the Day: By the time I got to work it was 11:00 am. Boss Kim said she was worried about what had happened to me and we discussed how variable my arrival times may be with this new schedule. I felt okay for most of the day at work, getting a little droopy towards the end of the day. Late in the afternoon my fuzzy brain got fuzzier. When my brain is fuzzy, it’s difficult to recollect and summon up at will specific small pieces of data. If I ask my brain to find the info, it’s like a slow librarian. She comes back with the data sometime in the future, when I’ve feasibly forgotten why I wanted it. The larger concepts and ideas are accessible, but the minutiae is off somewhere in a dense fog. So, when this phenomenon is occurring I can work successfully on writing or developing projects, but if the work has to do with detail work, I am very fuzzy. The fog is good for day dreaming or creatively imagining things but not much good for left-brain activities. That’s the way it seems to me.
Once I got home after work, I watched the news and then fell asleep for a 3-hour nap.
This experiment of going in for dialysis early in the morning, at first measure, is seeming to be too much for me. But, I have to do it on Thursday and Friday so I¹ll get more data points in order to see if it¹s just a time adjustment problem. I¹m going on Friday instead of Saturday this week because we are heading down to Kerrville on Friday for the first weekend of the Kerrville Folk Festival*.
*Online at http://www.kerrvillefolkfestival.com/
5/21/06
13) I hate Change
Synopsis Since Thursday: Liz and I discussed possibly changing to an early morning dialysis session. Kim (my boss) and I discussed the possible change. Theresa (my ED) and I discussed the possible change. Should I change? Should I stick with the way things are? Will the change be better for home? Will it be better for work? Will it be better for me? For Liz? For Shayna? What will be the benefit of changing my dialysis schedule? (According to the I Ching*, Decline [36] changing to Grace [22]). "Arghhhhhh!"
"I HATE CHANGE!" Change used to be cool, exciting, new & different, mysterious, adventuresome, and fun. But that was 35 years ago when I was a vagabond minstrel of “the Age of Aquarius” and the exploration of inner space, the final frontier, was our 5 year mission; to explore strange new worlds, create new tribes, and boldly go where no straight person had gone before. But now I’m way retired and love the stability of my little job and my little home and my little family. I’m like a hairy-footed hobbit, happy in my little hobbit house. “No need to change anything” says my fuzzy brain.
Back to reality: Even though we say in systems thought that 'change is constant', I don’t have to like it! So even the change of schedule of my dialysis is a problem for my fuzzy brain. I have to think about all the pro’s and con’s of it. If I change, it’ll be better for my work (Kim & I figured out), since I will have more ability to travel out of town. It’ll be nicer at home cause I can always be here in the early evening hours for dinner and family time (although Liz & I both know that is no guarantee we’ll eat before 8 anyway). On the down side, what about those times when Liz is out of town and I have to get Shayna to school? It’s much easier to get help with picking Shayna up in the afternoon than dropping her off in the morning. And, of course there is the consideration: do I really want to get up at 4:45 am three days a week? I got up at 5:30 for all the years my son had to catch a bus to his school across town and actually liked it! Maybe I’ll like it again.
El Milagro: Rosie cannulated me again today, again without much pain. The place was busier than usual, so I couldn’t come in until noon. I talked to Phyllis about my thoughts about changing to the early session and she offered that on those occasions when I can’t come in early, it is always easier to switch to a late session than it is to switch from a late session to an early session. That convinced me and I told her to move my name (on the big board) to the early session. She replied that I’ll start next Tuesday.
Data Notes: In @ 73.5 Kg and out @ 70.7 Kg.
*Wing, R. L. (2001) The I Ching workbook. New York: Broadway Books.
5/19/06
12) The Early Morning Edition
El Milagro: When I got here this morning at 5:40 am, the place was already jumping. I got hooked up in chair #17 by Rosie and almost immediately went back to sleep. (I¹m on first shift today so I could present at a TCFV conference this afternoon.) When I woke up at 9:15 Rosie was checking my machine and I ventured, "This would be perfect if there was coffee and breakfast served now". She laughingly replied, "You slept through the taco man. He comes every morning." Darn!
Upon observation (after waking up), I notice there are lots of men here on this first morning shift; and at least 7 of them could be workers. I only see a few women. Every chair is occupied. Phyllis stops by and, when I ask about her being here early, she tells me she gets here before 5:30 am and works until 5:30 pm. three days a week. Rosie was my tech today and she stuck me further up my arm than I¹ve ever been stuck: it was painless (without numbing medicine) even now, 3 hours later.
At the end of my session, as Rosie was de-cannulating me and I was tightly holding the gauze over my punctures, she mentioned that this chair (on first shift) is open and it could be mine if I want it. She continued that if I like it here early I should tell them I want this chair. I asked her hesitantly, "What happened to the person who left this chair? Did they die?". She replied with a chuckle, "So, you don¹t want a chair with bad mojo, huh? Well, the woman who sat here transferred to another shift... and we¹re happy she¹s gone cause she was trouble. You¹re no trouble so we¹d like to have you sitting here." Aha! She has her own agenda: getting easy old me into her section. I replied I would check it with work and Liz and get back to them. By the time I left, they had told Phyllis and she had stopped by to say it is okay with her if I change shifts. So, something new to consider after I've only been here 5 weeks. Originally staff had said that first session chairs hardly ever open up unless someone dies.
Data Notes: In @ 72.7 Kg and out @ 70.5 Kg.
5/17/06
11) Two Posts Today...
El Milagro: Today Michelle cannulated me and did a painless job, although the nurse had to come over later and re-stick me because the outgoing needle was “bottoming out”. With my minimal knowledge, I think bottoming out is where the needle is resting against the inside surface of the vein and thereby not drawing blood as well as it can. So, the nurse put in another needle and capped off the first one. She said they don’t like to withdraw it after I have received my Heparin, because it thins the blood and I would bleed too much if they took that needle out. So they just close the valve on it and tape it down until I’m done for the session.
Michelle is on dialysis too, which I didn’t even notice until she said my fistula looks like hers. Both were done by Dr. Settle, who seems to be the reigning artist of fistulas in Austin. Michelle does her dialysis at home with a machine she got through Medicare. But, she has to dialysize every night for nine hours…. I guess because the machine is much slower than these Cadillac’s we have here. Michelle has been on dialysis for 4 years now, and started because her Lupus worsened.
So, now I have 3 trocars in me and the last one was put in without the local anesthetic I usually get. Makes me feel like a real man! I was thinking recently about trocars, calling them turoks in my fuzzy brain. It seems to me that trocar sounds like an instrument that a Klingon would use. But now that I think more clearly, I guess ‘turok’ would be Klingon for truck.
Today there is a patient here somewhere in the maze who keeps saying “Help” in a faint, forsaken voice. The voice gives no hint of a gender; just a sense of desolation and weakness. These feeble “Help’s” emanate from some point in the room that I can’t readily see, so I can’t pin them to a person. But, it is curious that none of the staff seem to be going to the aid of the patient who says help. Finally, after about 20 “Helps” I hear a staff say, “Sandra; you don’t need anything.”, and I can’t see the staff either. A few minutes later the unidentified staff says, “You keep saying the same thing over and over Sandra.”. Sandra replies with a bit more life in her voice, “Shut up!”. Afterwards, it seems Sandra’s “helps” diminish although when I finally see her being rolled to her waiting son (my guess) in her wheelchair, she is again saying “Help……..Help……..Help” and her relative kindly says, “It’s okay. I’m taking you home now.” I, as many other patients I'm sure, was relieved that Sandra was being taken home by someone who loves her.
Notes: Weighed in at 71.9 and out at 71.3 Kg.
Tuesday (5/16)
El Milagro: As I was being cannulated by Kim and Tori today, Jennifer the Dietician was going over my “Detailed Nutrition” report (results of latest blood work). Kim and Tori were working together because Kim’s first attempt at sticking me found a clot in the needle, so Tori stepped in to find a better spot. According to Jennifer in reviewing my report:
& My albumin (protein) was good;
& My HCT CALC(HGBX3) is really good (that’s my red blood cell count btw);
& My IRON SATURATION is good;
& My FERRITIN is good (stored iron);
& My CALCIUM CORRECTED is good;
6 My PHOSPHORUS is very high and I must lower it by taking my binders and eating low phosphorus foods;
6 My CAxPHOS CORRECTED is also too high. Calcium + Phosphorus = Product. Again… take the binders.
So, Jennifer and I discussed my taking binders with every single morsel I put in my mouth: 5 with meals, 4 with ½ meals, 3 with snacks.
The only other thing of note was that I forgot my Dialysis Bag today so I had no earphones, no TV clicker, and no blanket. I had to be satisfied with a recent issue of Family Therapy Networker and my note pad…. but I didn’t really feel like writing. So, after reading awhile, I kinda laid there in semi-consciousness, listening to the hum of my bionic machine and the other various noises of a dialysis center.
Notes: In at 73.9 Kg. & out at 71.6 Kg.
5/12/06
10) Of Cannulation & Parathyroid Glands
El Milagro: I noticed on the way over here (west side of IH 35 South of Oltorf), driving through Zilker Park, just how brilliant green Austin is after all the rain we¹ve had. It is a perfect afternoon for doing something active outside. So, I breathe in the crisp air deeply for a few minutes while walking across the parking lot of my dialysis center. Kim again did a beautiful job of sticking me (the medical term is cannulation: the process of inserting a cannula, which is a flexible tube inserted to drain or administer fluid, ending with a trocar, a sharp pointed surgical instrument; i.e. needle). Phyllis reminded me of the term, spelled it, and exclaimed, “You’ve been cannulated, Jack” A few minutes later, as I am looking around doing my initial observation, I notice that Moritz is here. I remember to ask him if AB+ is a match for A+ for a kidney. Today we have 12 patients and 7 staff. Moritz is making his ‘rounds¹ like a high priest of the dialysis inquisition, and stops and as he watches me writing this he teases me about not having my laptop; "So, I thought you were the big computer guy. Where¹s your laptop?" to which I make some lame excuse like, "Since my infiltration I am not yet ready to move my arm enough to type but I¹m gonna bring it someday." Moritz and Ron the Nurse and Jennifer the Dietician discuss my recent blood work and Moritz says to put me on a new med for my overactive parathyroid gland. They also discuss my phosphorus still being high and ask if I am taking my binders at each meal, to which I say a confident "Yes!". They nod their heads thoughtfully and move on to their next victim, Jennifer saying over her shoulder, “I’ll be back”. Later Jennifer the dietician returns to more fully explain my para-thyroid situation, saying most of what I have copied below.
Parathyroid Glands*: There are four parathyroid glands which are normally the size and shape of a grain of rice. Occasionally they can be as large as a pea and still be normal. The four parathyroids are shown in this picture as the mustard yellow glands behind
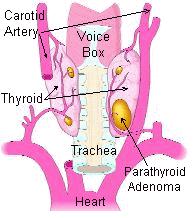 the pink thyroid gland. Normal parathyroid glands are the color of spicy yellow mustard. The ONLY purpose of the parathyroid glands is to regulate the calcium level in our bodies within a very narrow range so that the nervous and muscular systems can function properly. This is all they do. They measure the amount of calcium in the blood every minute of every day... and if the calcium levels go down a little bit, the parathyroid glands recognize it and make parathyroid hormone (PTH) which goes to the bones and takes some calcium out (makes a withdrawal from the calcium vault) and puts it into the blood. When the calcium in the blood is high enough, then the parathyroids shut down and stop making PTH. The single major disease of parathyroid glands is overactivity of one or more of the parathyroids which make too much parathyroid hormone causing a potentially serious calcium imbalance (too high calcium in the blood). This is called hyperparathyroidism. ….It is possible for a person to take too much vitamin D so that they absorb too much calcium from their diet and hold on to too much calcium in their kidneys... and their calcium goes high.
the pink thyroid gland. Normal parathyroid glands are the color of spicy yellow mustard. The ONLY purpose of the parathyroid glands is to regulate the calcium level in our bodies within a very narrow range so that the nervous and muscular systems can function properly. This is all they do. They measure the amount of calcium in the blood every minute of every day... and if the calcium levels go down a little bit, the parathyroid glands recognize it and make parathyroid hormone (PTH) which goes to the bones and takes some calcium out (makes a withdrawal from the calcium vault) and puts it into the blood. When the calcium in the blood is high enough, then the parathyroids shut down and stop making PTH. The single major disease of parathyroid glands is overactivity of one or more of the parathyroids which make too much parathyroid hormone causing a potentially serious calcium imbalance (too high calcium in the blood). This is called hyperparathyroidism. ….It is possible for a person to take too much vitamin D so that they absorb too much calcium from their diet and hold on to too much calcium in their kidneys... and their calcium goes high.After rounds, Moritz was working on the computer for awhile, but then, before he left he completed another sweep of the patients, having brief, more sociable conversations with them as he goes. He has an optimistic bedside manner as he explains medications, encourages people to eat a healthy diet (in Spanish), and kids with those who can. With Mr. Animado Moritz jokes about his coming in late, saying “You don’t work” when he says he is late because of working. As usual, Mr Animado is in good and noisy spirits. Shortly afterwards, I look around and Moritz is gone. Later in the session, Ron the Nurse visits with Mr. Animado, asking him if they can find a better center for him to go to and by the end of the evening, Mr. Animado is transferred to another center. I’m not sure that Mr. Animado wanted that…. it seems the Milagro staff had had it with his coming in late. Maybe there is more to this story; I just report it from my perspective. Obladi Oblada life goes on.
Weighed in at 72.2 Kg and out at 71.4 Kg
*Norman Endocrine Surgery Clinic (2006) Introduction to parathyroid glands. Retrieved online May 12 from http://www.parathyroid.com/parathyroid.htm
5/10/06
9) Dialysis & Sleep
El Milagro: Just another dialysis session... boring today. Weighed in at 72.9 and out at 72.0.
Later: After dialysis, when I get home, I am usually somewhat drained. I get home, eat dinner, and then generally "rest on the couch", which means I watch some TV or take a nap. Couch-napping is a family tradition in the Nowicki family. When I was a child my dad would frequently come home from work, eat dinner, and sack out on the couch in front of the TV. My son sacks out on the couch when he is here and has nowhere to go. My brother used to sack out and probably still does.
So, anyway, I feel kinda drained when I get home. The night after a dialysis session I sleep better than I have in years! For the last few months before I started dialysis I was having terrible sleep. I couldn¹t get to sleep early; I woke up three or four times to urinate; and I had bad fidgety legs that got me up and wandering around the house in the dark. After dialysis I sleep like a bear in the dead of winter and have vivid dreams. In the morning I awaken groggily and after my coffee I begin to feel great. Feeling great is a blessing!
5/7/06
8) Of Cybernetics, Morphic Fields, & AV Fistulas
On Saturdays I am supposed to call in to the center in the morning to see if they can fit me in early. Today I called and Kim answered the phone. I identified myself and she asked when I’d like to come in. I replied, “10:30” and I heard Phyllis in the background saying “11. Tell him he’s got a deal for 11.”. I like this idea of flexibility on the weekend. Today I’ll get outa there by 3 in the afternoon!
On another note, I got an email from my friend Martha on the 2nd. In response to my blog, she said, “I’m sending you loads of Light and will check your blog often”. The more people that know of my situation, the more people there are hoping, praying, visualizing, and desiring my healing and continuation in life. This is a good reason to write this blog and be open and loquacious about my dis-ease and my medical situation. I have friends who, when we get together, we share our health progress and regress with each other as a matter of friendship. However, some people want to keep their medical situations private and are reluctant to discuss them with anyone else. I also have friends like that. They have their health conditions and won’t discuss them openly for some reason that I don’t really comprehend. It may be that they simply don’t see our friendship as being close enough to share those things. Or, they may be in some form of denial.
In my trainings I frequently say “Denial is a river in Egypt!” (allegedly from Mark Twain) to suggest that denial doesn’t really exist. It’s preferable for us to think of it as ‘suppression’, because suppression is a choice of the beholder. When people choose to put information about their situation out into the world, it helps them to accept their situation as well as to receive support and focused healing energy from their friends (system) and humanity (larger system).
When we understand ‘humanity’ as a system, and we apply concepts from cybernetics, like recursion (reciprocal causality), autopoiesis (self-generation), and morpogenisis (growth of the system), we find that the larger system influences the individual just as the individual impacts the larger system (see Ray Becvar’s books*). In the larger system there is a collective memory which we, as humans can ‘tune in’ to. This collective memory exists as morphic fields according to Rupert Sheldrake**. These morphic fields are “non-material regions of influence extending in space and continuing in time. They are localized within and around the systems they organize”. So, the information we put out into the world (larger system) about our health situation is available for human consumption and consideration (hope, prayer, visualizing, creation, etc.) and these considerations recursively influence the morphic fields such that they have a postive resonance (impact) on all parts of the individual system.
That’s the way I see it! Thanks Martha for sending in the Light.
* Becvar, D.S. & R.J. (1982) Systems theory & family therapy: A primer. University Press of America: Lanham, MD.
** Sheldrake, R. (1988) The presence of the past: Morphic resonance and the habits of nature. Times Books: New York.
El Milagro: James hooked me up this morning and it was interesting to see how each new tech that prepares me has their own way of doing this process. I mentioned to James that I think I am supposed to still be on small needles (he checked the chart and agreed) so he decided to use size 17 needles. He explained that they use smaller needles until my fistula toughens up. He also set a tourniquet because my vein seemed to be on the verge of collapsing today (who knows why that happens?).
Today I am seated on the periphery of the pattern of chairs, in a corner where it appears they decided at some point to put an extra chair to get just one more person into the mix. This chair faces the back of the nurses command center; so I can see what they are doing behind the desk. When I was a kid, I always used to wonder how life was behind the counter when I went into stores, restaurants, and other facilities. Now I feel a bit of nostalgic excitement at the chance to see behind the counter. Behind the counter right now are four nurses (Phyllis, Ron, Connie, and Kim). Kim is transferring info from patient’s daily logs onto a computer. Ron seems to be preparing doses of the various injections patients machines get during their dialysis. He fills the hypodermic needles, checks them carefully against a form, ensures they have no air in them, and then puts them in a rack to be distributed around the center. Only the nurses give these shots to the tubes connected to the patients. According to Connie, the shots I get each time are Venofor (iron), Epogen (Procrit), and Zemplar (for my bones).
Throughout my session today, my machine frequently beeped crazily and someone had to come quell the beeping and adjust the flow rate to keep my vein from collapsing. After several attempts by Tori at readjusting the needle from my fistula to the machine. Tori shared with me that James should have used size 16 needles, which are the ones I formerly used before Tori gave me size 15 last time. He concluded that I should tell the tech to use size 16 for the time being. Finally Connie solved the flow problem by putting extra gauze under the needle to push it down into the middle of the vein because she thought it was resting against the inside wall of the vein, thus interrupting good blood flow. There were no further difficulties and I got out of there by 4:15 pm.
Data Notes: I weighed in at 72.3 Kg. and out at 70.6 Kg. (1Kg. = 2.2 lbs.).
Definitions: I think I offered several posts ago to put in some information about my fistula that buzzes for the uninitiated who touch it.
AV fistula*:
AV (arteriovenous) fistulas are recognized as the preferred access method. To create a fistula, a vascular surgeon joins an artery and a vein together through anastomosis. Since this bypasses the capillaries, blood flows at a very high rate through the fistula. One can feel this by placing one's finger over a mature fistula. This is called feeling for "thrill", and feels like a distinct 'buzzing' feeling over the fistula. Fistulas are usually created in the non-dominant arm, and may be situated on the hand (the 'snuffbox' fistula'), the forearm (usually a radiocephalic fistula, in which the radial artery is anastomosed to the cephalic vein) or the elbow (usually a brachiocephalic fistula, where the brachial artery is anastomosed to the cephalic vein). A fistula will take a number of weeks to mature, on average perhaps 4-6 weeks. During treatment, two needles are inserted into the fistula in opposite directions, one to draw blood and one to return it.
The advantages of AV fistula use are lower infection rates,as there is no foreign material involved in their formation, higher blood flow rates (which translates to more effective dialysis), and a lower incidence of thrombosis. The complications are few, but if a fistula has a very high flow in it, and the vasculature that supplies the rest of the limb is poor, then a steal syndrome can occur, where blood entering the limb is drawn into the fistula and returned back to the general circulation without entering the capillaries of the limb. This results in cold extremities of that limb, cramping pains, and if severe, tissue damage.
* Answers.com (2006) Retrieved online May 7th from http://www.answers.com/topic/hemodialysis?hl=fistula&hl=vein
5/5/06
7) It Started with Synthroid
El Milagro: Tory hooked me up with larger needles today, so it was a bit painful getting stuck. While he was jabbing me, I wondered aloud why it hurt and was it larger needles, to which he replied, “Oh. I thought you were up to larger needles already”. Later when he saw me making these notes, he offered that his name is spelled with an ‘i’ because in Japanese Tori means ‘bird’. The things that we learn when we listen to our environment!
As Tori was finishing up taping my tubes down so I don’t pull them around, Marilyn and Phyllis were talking to me about finalizing my plans for Memorial Day weekend. Their suggestion, since the center in Kerrville isn’t open on Saturdays, is that I come in here early Friday (5:30 – 9:30 am) and then back again at 3:30 pm on Monday. So, I’ll have my regular dialysis on Thursday, then again on Friday morning and then skip two days until Monday. Then I skip Tuesday and go back on the next Thursday. I am sure this paragraph is captivating for most readers… as it reflects the mundane scheduling work that we must all go through in our busy lives. As we read it, we are probably all saying, “Ah yes, I can totally identify with this minutiae”.
There are about 6 patients here right now, and 7 staff. The staff kind of circulate through the place, checking on the progress of the machines and writing some numbers on the patients daily log which is kept on a clipboard on top of the machine. I am sure there is a staff responsible for each chair, but as they circulate, it seems they all check the machines and write on the log. Sometime during each time I am there, each staff will come up and greet me formally and ask how I am doing today. I get the idea they are hyper cautious and that makes me feel good.
There is an older, non-ambulatory Hispanic woman who always finishes up her session sometime after I arrive. Today she is in a chair directly across from me, so I get a good view of her. She is always accompanied by her adult daughter (I believe), who sits with her devotedly throughout her dialysis, giving her snacks, adjusting her covers, shifting her around in her chair to make her more comfortable, talking to her, and being her translator with the English-speaking-only staff. The younger woman is deferential with the older woman and yet she also seems to have great influence on the older woman. This seems to be a symbiotic relationship they have worked out over a long period of time. The older woman seems resigned to her fate but she isn’t going down quietly. She grumbles, in a whispering voice, her complaints and objections to the younger woman and the younger woman works to calm them. This scene reminds me of all that I’ve read about the baby-boomers beginning to care for their parents and having to adjust their typical communication styles to continue the parent/child dialogue.
As a formerly ‘healthy’ person who had little contact with the medical establishment, it is quite perplexing to be so concerned now with my health. For years I only had one doctor and I usually only saw him for physicals and the annual bout with cedar fever. When I took meds it was limited to a specific condition and didn’t last long. And then, in my forties I developed a lazy thyroid and began my slide into the world of pharmaceuticals. It started with Synthroid! At first it was difficult to remember taking my daily synthroid. After meeting Moritz, in ’98 I had to buy one of those plastic pill boxes (that I associate with ‘old’ people) for my 6 daily doses. By the time I started dialysis I was up to 14 different pills a day and thinking of myself as an ‘old’ person. Now, fortunately the machine helps with my meds and I am back down to 9. Another advantage of being on dialysis!
5/3/06
6) Phosphorus News
El Milagro: Today Kim hooked me up smoothly. She was the tech who hooked me up on my first day, and she is always conscientious about telling me to keep my arm still, and she asks how I feel a lot.
I had a medium long conversation with Jennifer the dietician today. She arrives asking if I am taking my binders with every meal. The binder (Renagel 800 mg) attaches to phosphorous in my intestinal tract and escorts it out of my body ( Patients on dialysis should keep their phosphorus levels in the 3.5 to 5.5 mg/dL range). Without such an escort, phosphorous builds up because neither kidney nor dialysis machine can process it.
According to Jennifer, my last blood work showed high phosphorous again so we were trying to figure out when I started taking the Renagel and she was curious about whether I am taking it with every meal…. I assured her I am. Other than that, she reported that my blood work looked good. We were also talking about my adjustment to dialysis and I ended up hesitantly telling her about my blog, which she was immediately curious about. She asked for the web address and I reluctantly gave it to her, cursing myself for my being so acquiescent in the presence of engaging young women. So, the cat is out of the bag in this system and I hope that it takes awhile to become common knowledge, and thus pull me into the box.
The place is not crowded today… I can see the whole room and there are only 8 or 9 chairs occupied. There are 11 staff here, so I think that is a good client/staff ratio. Marilyn social worker stopped by and we discussed her efforts to get me a visit to the Kerrville Dialysis Center for Saturdays during the Kerrville Folk Festival. She said she will talk to the right person down there tomorrow. I shared that I had also put in an online request for space through Davita.
Got out of there by 7:45 tonight.
Later:
Some High Phosphorus Foods
Milk, Cheese, Yogurt, Ice Cream, Beer, Cola, Milk-based Coffee and Chocolate Drinks, Chocolate, Brown Rice, Wild Rice, Whole Grain Breads, Cereals & Crackers, Corn Tortillas, Pancakes, Waffles, Biscuits, Pizza, Avocado, Nuts, Seeds, Nut butters, Dried Beans & Peas, Corn & Peas, Processed Meats (Hot Dogs, Sausage, Turkey Sausage, Bologna), Sardines